Tuesday 20 May 2025
Researchers have made significant strides in understanding the factors that contribute to hospital resource utilization, specifically identifying demographic, lifestyle-related, and socioeconomic characteristics that increase the likelihood of patients seeking medical attention.
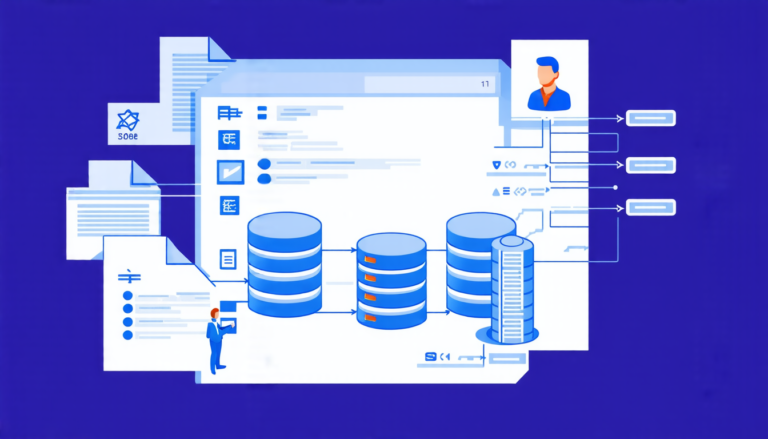
The study analyzed data from the National Health and Nutrition Examination Survey (NHANES) spanning 17 years, focusing on a vast array of variables including demographics, dietary habits, health examination results, laboratory findings, and questionnaire responses. The researchers employed a DevOps framework to integrate continuous integration and deployment practices into their analysis pipeline, allowing for seamless updates and adaptability.
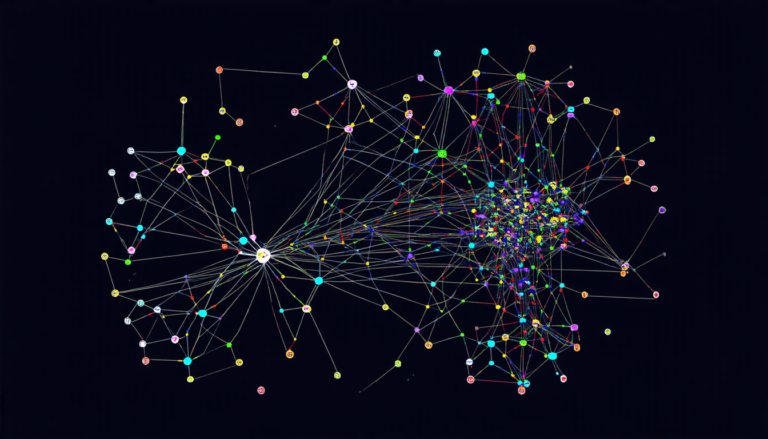
The findings revealed that demographic characteristics such as age, gender, and race play significant roles in hospital resource utilization. Specifically, older adults (60+ years) and non-Hispanic black individuals were found to be at a higher risk of utilizing hospital resources. Additionally, socioeconomic factors like education level, income, and health insurance status also emerged as important predictors.
Lifestyle-related characteristics, including dietary habits and physical activity levels, also significantly contributed to the likelihood of hospital resource utilization. Patients who consume high amounts of energy-dense foods, sugar, and saturated fats were more likely to require hospital care. Furthermore, individuals with a history of smoking, heart disease, and diabetes were at a higher risk of utilizing hospital resources.
Notably, anxiety status was found to be a significant predictor of hospital resource utilization, particularly in recent years. This highlights the importance of mental health services and stress management in reducing healthcare burdens.
The study’s results also underscore the critical role of socioeconomic factors in determining access to healthcare. Patients without health insurance or with lower socioeconomic status were less likely to utilize hospital resources, emphasizing the need for targeted interventions aimed at improving healthcare equity.
This comprehensive analysis provides valuable insights into the complex interplay between demographic, lifestyle-related, and socioeconomic factors that influence hospital resource utilization. By understanding these predictors, policymakers can develop more effective strategies to address healthcare disparities and optimize resource allocation. The researchers’ innovative approach to data analysis using DevOps principles further underscores the importance of integrating cutting-edge methods in medical research.
The study’s findings have significant implications for healthcare policy and practice. By targeting high-risk populations and addressing socioeconomic barriers to care, policymakers can reduce hospitalization rates and improve health outcomes. Furthermore, healthcare providers can use this information to develop more effective treatment plans and interventions tailored to individual patient needs.
Cite this article: “Unlocking the Complexities of Hospital Resource Utilization: A Multi-Faceted Analysis”, The Science Archive, 2025.
Hospital Resource Utilization, Demographic Characteristics, Socioeconomic Factors, Lifestyle-Related Characteristics, Diabetes, Heart Disease, Smoking, Anxiety Status, Health Insurance, Healthcare Equity